Radiotherapy is an essential part of cancer treatment but what is the current status in Kenya? We took a look at how Kenyatta University Teaching, Referral & Research Hospital (KUTRRH) have taken steps to offer patients advanced radiotherapy in Kenya with the CyberKnife® System.
Cancer Burden in Kenya
Cancer is the third leading cause of death in Kenya after infectious disease and cardiovascular diseases1. The annual incidence of new cancer cases increased from 37,000 to 47,887 between 2012 – 20181, and are expected to continue to rise. With a population of 54.7 million nearly 23% of sick patients do not pursue healthcare due to several barriers, including high costs, the need to travel long distances and a lack of healthcare education and awareness1. Sadly, even to date the majority of cancer patients only seek treatment when the disease is already advanced, contributing to high mortality rates2. In Kenya, 60% of patients with cancer are less than 60 years old3.
What is the Status of Radiotherapy Services in Kenya?
Between 2009-2021, six private hospitals and three public hospitals opened facilities for cancer care and treatment, including radiotherapy services. The majority of workload remains at public institutions where costs for cancer are more affordable compared to private hospitals.
Kenyans can apply for the National Health Insurance Fund (NHIF) to help cover the cost of their cancer treatments, including radiotherapy. In 2019, a commitment was made to strengthen efforts to address cancer as part of universal health coverage4. And, now there is a ‘National Cancer Control Strategic Plan 2023-2027’ in place with a focus on cancer prevention, strengthening primary based healthcare and community health interventions as well as digitalization of cancer services. One of the goals of this strategy is to ensure the timely initiation of comprehensive treatment, strengthening access to quality sustainable care and improving the quality of life for cancer patients.
Bringing advanced radiotherapy to KUTRRH with the CyberKnife System
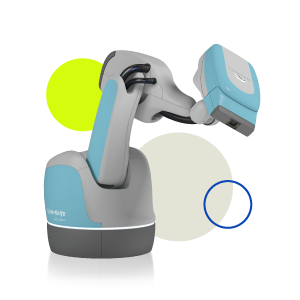
In September 2023 Kenyatta University Teaching, Referral & Research Hospital (KUTRRH) treated their first patient on the CyberKnife® System. The vision was to create a Centre of Excellence in oncology by providing end-to-end diagnosis and cancer treatment options at KUTRRH. While the hospital has a linac and brachytherapy suite for the treatment of cancerous tumors, there was a need to move into high precision radiotherapy treatment and hence the government supported the acquisition of a CyberKnife System. This decision was made to decrease outbound medical tourism and increase inbound medical tourism. Now patients can experience world-class treatment at KUTRRH’s CyberKnife Centre.
Interview with Ruth Manyagi at KUTRRH

We interviewed Ruth Manyagi, Manager of the CyberKnife Centre at KUTRRH to learn how patients access radiotherapy in Kenya and how the CyberKnife System has changed their radiotherapy department
Kenya is a developing country in Africa, with a GDP of $110,519 million in 2021, ranking Kenya the 7th country in Africa. In 2020, there were 42,000 new cancer cases diagnosed and 27,000 cancer related deaths. Due to late presentation the mortality rates are high. At KUTRRH radiotherapy centre we predominantly treat cancers of the prostate, esophagus, cervix, breast, rectum, head and neck and lung. We often treat more advanced stages of disease because of late presentation.
How easy is it to access radiotherapy in Kenya?
For those patients who are Kenyan and employed, they can apply for NHIF, where the government contributes towards treatment, including radiotherapy on the CyberKnife System. But, one of the issues is that not everyone is registered with NHIF. For many Kenyans they do not have the means to pay for basic needs and are unable to apply for NHIF. For these people they often fall into a situation where they are unable to afford treatment and often rely on help from others including funding from hospitals. There are private hospitals available, but they are much more expensive than the government hospitals.
Another factor that leads to problems accessing care is that NHIF will contribute to cancer treatment but no other supportive needs like travel or accommodation. If patients are travelling from far away it becomes very difficult for them to gain access to treatment when needed and contributes to late presentation of their disease.
Lack of education and awareness of cancer is also a major hurdle. Unfortunately, many people do not know what symptoms or treatment options are available and therefore they just don’t know what to do.
How far do people come to your center?
Kenya is very densely populated, with most people living outside of the capital city of Nairobi in villages. Some patients travel a very long distance to receive their treatment. For example, some people will travel three days to come to KUTRRH to receive radiotherapy.
How many patients receive radiotherapy daily at KUTRRH?
KUTRRH is one of the biggest government hospitals in Kenya. At the moment we have just 1 conventional linac, a brachytherapy unit and the CyberKnife System. On the conventional linac we treat 100 patients per day. We have three shifts of staff spread out from the morning until midnight when the last patient is treated.
What was the reason behind purchasing a CyberKnife System?
One of the reasons for purchasing a CyberKnife System was to be able to provide treatments that were not available in Kenya. Now, with the CyberKnife System we are able to treat patients with intracranial lesions, including meningioma, arterial venous malformations (AVM), acoustic neuromas and other cancerous and benign conditions in the brain and spine. We also treat inoperable intracranial tumors, where surgery was not possible due to the location of the disease or because in some situations the patients refuse surgery.
Before the CyberKnife System was installed a lot of these patients were treated abroad, in parts of Europe and India. But the government wanted to improve access to these patients in Kenya and from surrounding areas, so now with the CyberKnife System patients can receive this treatment more easily. Our CyberKnife System is the second system in Africa. So, we are expecting patients to be coming from other surrounding countries like Ethiopia, Somalia, Sudan, Tanzania, Nigeria. and other countries in Africa.
We can also treat patients with fewer fractions, for example we can now treat people in 5 treatments compared to 30 treatments. This helps to reduce the cost to the patients that are coming far from home, and is one of the reasons now that patients come to KUTRRH for their treatment. Due to the high precision of the CyberKnife System we are also able to treat with smaller treatment margins which helps to improve outcomes such as better tumor control and reduced side effect for the patients.

What was it like to get a team together to work on the CyberKnife System?
One of the main agendas when introducing the CyberKnife System was to ensure we had a qualified team to run the unit. I was trained on the CyberKnife System before coming to KUTRRH so I was able to help support the team. But for most there was no expertise in this area. Accuray were really supportive to us from commissioning to treating the first patient. They didn’t just come and go, even now they help us if we are stuck with something, and we are very grateful for that.
Some of the doctors, physicists and radiation therapists were sent to India for their training to learn how to operate and utilize the CyberKnife System. It was a big change for us at KUTRRH, and there was a lot of training. But it was important for us to have gradual training to become confident in different treatment delivery techniques including real-time tracking with Synchrony®.
What are the future aspirations of the CyberKnife System at KUTRRH?
As we have more time on the CyberKnife System our expertise will increase, and we are hoping to treat more intracranial cases and extracranial cases. At the moment Kenya does not have anyone qualified in prostate fiducial marker insertion and we are currently looking for someone to help with this so we can start to treat prostate cancer patients. Prostate cancer patients make up the highest number of patients we treat with radiotherapy at KUTRRH. There is a long waiting list, and we believe we could help to treat these patients on the CyberKnife System.
We also need to make sure that there is awareness in Kenya of the CyberKnife System. People need to be aware as well as referring clinicians that this system is available to help ensure more people have access to it.
After the first couple of months we successfully treated 80 patients and we know we have capacity to treat more. When we are able to treat prostate cancer patients we know the numbers will shoot up and we will be celebrating that once we have someone to help us with the fiducial marker insertion.
In one way or another, cancer will affect us all. And it has immense impact on patients and their families as well. In Kenya, we are so proud to have the most modern device, the CyberKnife System, from Accuray in our oncology department. The CyberKnife System has the ability to track the treatment in real-time, ensuring high level of precision, and it delivers stereotactic treatments for a range of different sites, such as lungs, prostate and other metastatic diseases, which, right now we are dealing with in Kenya. And, although there are various oncology treatments, having the opportunity with the CyberKnif® System allows us to work with smaller margins, allowing complete precision and lower toxicity levels to the patient. So here in Kenya, it will give us an opportunity to generate income through private and overseas patients. The CyberKnife System is a well-known non-invasive treatment which we hope will attract more patients here in Kenya, mostly from overseas and also, the neighboring countries and also our own Kenyan people.’
Ruth Manyagi
References
- Pankaj, G et al. (2021) Cancer on the Global Stage: Incidence and Cancer-Related Mortality in Kenya. WORLD HEALTH ORGANIZATION REGION: AFRICA. The ASCO post. Available at: https://ascopost.com/issues/february-25-2021/cancer-on-the-global-stage-incidence-and-cancer-related-mortality-in-kenya/
- Nydone et al. (2022) Current Status of Radiotherapy Services in Kenya. Scientific Research. Available at: https://www.scirp.org/journal/paperinformation?paperid=116852#t1
- Makau-Barasa et al. (2017) ‘Improving access to cancer testing and treatment in Kenya’ American Society of Clinical Oncology. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6180746/pdf/JGO.2017.010124.pdf
- Ministry of Health Kenya ‘The National Cancer Control Strategy (2023-2027). Available at: https://www.iccp-portal.org/system/files/plans/NATIONAL%20CANCER%20CONTROL%20STRATEGY%202023-2027_compressed.pdf
The views contained and expressed in this blog, are those of the author and do not necessarily reflect the views or policies of Accuray Incorporated or its subsidiaries. No official endorsement by Accuray Incorporated or any of its subsidiaries of any vendor, products or services contained in this blog is intended or should be inferred.